Prostate Cancer
The prostate is a gland in the male reproductive system. It lies just below the bladder (the organ that collects and empties urine) and in front of the rectum (the lower part of the intestine). It is about the size of a walnut and surrounds part of the urethra (the tube that empties urine from the bladder). The prostate gland makes fluid that is part of the semen.
Prostate cancer is most common in older men. In the U.S., about 1 out of 5 men will be diagnosed with prostate cancer.
- Prostate cancer is a disease in which malignant (cancer) cells form in the tissues of the prostate.
- Signs of prostate cancer include a weak flow of urine or frequent urination.
- Tests that examine the prostate and blood are used to detect (find) and diagnose prostate cancer.
- Certain factors affect prognosis (chance of recovery) and treatment options.

The prostate is the gland below a man’s bladder that produces fluid for semen. Prostate cancer is common among older men. It is rare in men younger than 40. Risk factors for developing prostate cancer include being over 65 years of age, family history, and being African-American.
Symptoms of prostate cancer may include:
- Problems passing urine, such as pain, difficulty starting or stopping the stream, or dribbling
- Low back pain
- Pain with ejaculation
To diagnose prostate cancer, you doctor may do a digital rectal exam to feel the prostate for lumps or anything unusual. You may also get a blood test for prostate-specific antigen (PSA). These tests are also used in prostate cancer screening, which looks for cancer before you have symptoms. If your results are abnormal, you may need more tests, such as an ultrasound, MRI, or biopsy.
Treatment often depends on the stage of the cancer. How fast the cancer grows and how different it is from surrounding tissue helps determine the stage. Men with prostate cancer have many treatment options. The treatment that’s best for one man may not be best for another. The options include watchful waiting, surgery, radiation therapy, hormone therapy, and chemotherapy. You may have a combination of treatments.
Better treatment
Prostate cancer is the second most common cause of cancer deaths in males and will afflict 1 in 6 men.
Many diagnostic prostate biopsies fail to detect occult cancers because of the difficulty in properly determining the prostate’s anatomy. Approximately 20% of ultrasound image guided prostate biopsies return negative results despite rising levels of prostate-specific antigen (PSA) markers in the blood and the presence of cancer somewhere in the 30+ cc gland. These failures have been attributed by some to the hesitation to sample one of the two major parts of the glands— namely the predilection toward the more easily reached peripheral zone (PZ) over the less accessible central gland (CG). We can outline these two non-overlapping adjacent regions of the gland.
Advancing solutions to this vexing clinical problem will raise awareness about the impact computer image processing can have toward addressing a widespread, critical healthcare puzzle. Open and closed source algorithms applicable to both 1.5T and 3T magnetic resonance images (MRIs) will be most welcome.
MRI of the Prostata gland
The magnetic resonance imaging (MRI) of the prostate gland is the most accurate method to diagnose and confirm prostate cancer requiring treatment. Detection of prostate cancer requiring treatment is more sensitive using the MR technology than the methods used so far, and this test either rules out or confirms particularly the aggressive cancers that have a high mortality. In many cases today, the MRI of the prostate gland can be used for detailed diagnosis as an alternative to biopsy, the surgical removal and testing of the relevant tissue. The investigation gives the following results:
- the existence of prostate cancer
- the exact location and size of the cancer focus
- the spread and growth in the peri-prostatic area
- the monitoring of growth and aggressiveness of cancer detected (active surveillance)
- structured reporting according to the PI-RADS classification.
This gives the urologists a precise indication for further diagnostics such as a targeted puncture and treatment of the disease.
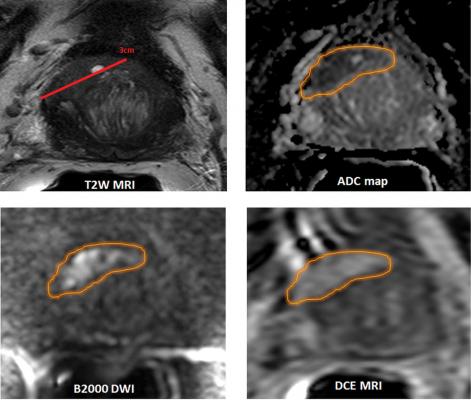
Multimodal Diagnostics in MRI
Besides the high-resolution image of the prostate gland, the methods of diffusion-weighted imaging (DWI) and the dynamic perfusion-MRT are also used to determine the aggressiveness and the spread of a probable tumor as accurately as possible.
The high field-MRI-spectroscopy is a functional testing method that also contributes to the diagnosis. This determines the relationship between various products of metabolism in the prostate, thus giving more information about the existence of a prostate cancer.